One important issue that my team and I encounter time and again comes from our potential customers.
We live in Spain and deal intensively with water and its treatment into drinking water.
We meet a lot of people at trade fairs and others come to our showroom in Palma de Mallorca, where they can enjoy freshly filtered water from the tap at our water test centre.
The water in Palma is usually highly chlorinated and therefore undrinkable.
We explain to people that this water contains high levels of minerals and that it remains so even after it has been filtered by our filter systems.
Our drinking water filters work selectively and only remove the negative substances such as chlorine, heavy metals and many others.
Well, many of these people now suddenly said that calcium in water is not good, even dangerous.
Yes? …. and we ask why?
They say that if you drink water with calcium in it, it will damage your kidneys.
We are always completely astonished, because we know that this is not true. And we ask who said that.
The answer usually comes out like a shot, my doctor!
In fact, we are always slightly shocked and ask how? Surely that can’t be true?
I would like to emphasise that we have experienced this very often.
We don’t know to what extent people’s perceptions correspond to actual statements made by doctors.
We don’t want to and can’t judge that!
But we would very much like to contribute to clarification.
So I spent a long time thinking about how to prepare and present the topic.
I’ve read a lot and talked about it with doctor friends.
But also with someone who specialises in holistic health.
In Germany, he runs the ‘Academy for Human Medicine’, – Frank-Joachim Ehling
Quote on the homepage:
Holistic health is the feeling of unity and co-operation of body, mind and soul – the experience of all-encompassing well-being and vitality.
With personalised nutritional advice, we support you in the prevention of osteoarthritis, strengthen your immune system and promote the body’s natural detoxification.
For more energy, balance and quality of life.
I told him my concerns and he was immediately willing to write for us on the subject of calcium.
So I am very happy to present to you here what Frank-Jochaim Ehling has to say about it.
It is not only very informative, but also very exciting!
https://www.ganzheitlichgesund-borken.de/
Calcium is a true all-rounder in our body.
It not only ensures strong bones and teeth, but also plays a key role in muscle contraction – from heartbeat to movement. It also supports blood clotting by promoting wound healing in the event of injuries.
Calcium is also involved in signalling between nerve cells and helps to regulate important processes such as hormone balance. Without this essential mineral, our bodies would literally falter!
The role of mineral water as a source of calcium compared to solid food depends on several factors:
1. The calcium content of the water
2. The daily amount drunk
3. and the intake through food.
Here is a clear analysis:
Calcium from mineral water:
Content: The calcium content varies greatly depending on the brand. Some mineral waters (e.g. Gerolsteiner) contain up to 300-400 mg calcium per litre, others only 10-50 mg/L.
Bioavailability: Calcium from water is absorbed very well, often better than from some plant foods (e.g. spinach), as it contains no inhibitors such as oxalic acid.
Example: 2 litres of calcium-rich water (e.g. 350 mg/L) could provide around 700 mg of calcium per day. The recommended daily requirement for adults is around 1000 mg (according to the DGE) and can vary depending on age and gender.

Calcium from solid food:
Sources: Dairy products (e.g. cheese: 500-1000 mg/100 g, yoghurt: ~120 mg/100 g), green vegetables (e.g. broccoli: ~50 mg/100 g), nuts (e.g. almonds: ~250 mg/100 g) or fortified products are the main sources.
Amount: A typical diet with dairy products often covers 500-800 mg of calcium per day, but can be significantly lower (e.g. 200-400 mg) with a vegan diet or low consumption.
Bioavailability: Variable – dairy products offer high absorption (approx. 30-40%), while plant sources may be limited by substances such as phytic acid or oxalic acid (10-20%).
Proportion: In a balanced diet with dairy products, solid food usually provides the majority of calcium (70-90%). Mineral water can then contribute 10-30%.
With a vegan diet: Mineral water is often more important here, as plant sources provide less calcium and the intake is lower. A calcium-rich water could then cover 50-70% of the requirement.
Practical:
If someone drinks little water or only low-calcium tap water (often <50 mg/L), the main burden remains with the diet. Conclusion: Mineral water can play an important supplemental role, especially when calcium intake from food is low or needs are high (e.g. pregnancy, risk of osteoporosis). It does not replace solid food, as this often provides more complex nutrients, but calcium-rich water (e.g. >200 mg/L) is an easy way to optimise supply – especially if the diet is not ideal.

Calcium levels in the body can be measured in different ways:
– in whole blood (or serum/plasma)
– in tissue (e.g. hair).
Both methods differ in their significance, purpose and interpretation.
Calcium in whole blood (serum/plasma):
What is measured? As a rule, calcium is tested in blood serum or plasma, not in whole blood, as most of the calcium is dissolved in the blood (ionised or bound to proteins). Typically, the total calcium value (approx. 2.2-2.6 mmol/L or 8.8-10.4 mg/dL) or the ionised calcium (approx. 1.1-1.35 mmol/L) is determined.
Significance:
Reflects the current calcium level in the blood, which is strictly regulated (homeostasis by hormones such as parathyroid hormone and vitamin D).
Shows acute changes, e.g. in the case of parathyroid disorders, kidney function or vitamin D deficiency.
Approx. 99 % of the body’s stores are in bones, only 1 % circulates in the blood – the laboratory value therefore says little about the total stores.
Purpose: Diagnosis of diseases such as hypercalcaemia (e.g. tumours) or hypocalcaemia (e.g. vitamin D deficiency), monitoring of dialysis patients or acute conditions.
Advantage: Fast, standardised, clinically well validated.
Disadvantage: Does not reflect the long-term supply or stores in the body.

Calcium in tissue (e.g. hair mineral analysis):
What is measured? The calcium content in hair is determined using special analysis methods (e.g. mass spectrometry). Hair grows slowly (approx. 1 cm/month), so the value shows an accumulation over weeks to months.
Significance:
Should reflect the long-term calcium supply or mineral balance in the body, including possible deposits or imbalances.
Can provide indications of nutrition, metabolism or chronic deficiencies/excesses.
Often considered in relation to other minerals (e.g. magnesium, zinc) to interpret ‘stress patterns’ or ‘mineral imbalances’.
Purpose: Used primarily in alternative medicine or nutritional counselling, e.g. to identify trends in mineral intake or to investigate environmental pollution (e.g. heavy metals).
Advantage: Non-invasive, could show long-term patterns.
Disadvantage: Scientifically controversial – the results are difficult to standardise as they are influenced by external factors (shampoo, colouring, environment) and have no direct correlation to blood values or bone stores. Not recognised as a diagnostic tool in conventional medicine.
Comparison:
Temporal aspect: Blood shows the momentary state (‘snapshot’), hair a historical perspective (‘long-term protocol’).
Regulation: The calcium level in the blood is closely controlled by the body (bones as a buffer), whereas hair tends to reflect passive deposits that are not actively regulated.
Relevance: Blood values are crucial for acute medical diagnoses (e.g. cramps due to hypocalcaemia). Hair analyses are speculative and intended more for preventive or holistic approaches.
Accuracy: Blood tests are precise and clinically validated; hair analyses are subject to interpretation and less reliable.
Example:
Blood: A value below 2.2 mmol/L could indicate an acute deficiency (e.g. hypothyroidism), even if the bone stores are full.
Hair: A high calcium value could indicate excessive intake (e.g. supplements) or deposits, but says nothing about the current blood level.

Conclusion:
Blood testing is the gold standard for checking functional calcium status, while hair analysis provides complementary, but possibly uncertain, evidence of long-term trends at best.
For health problems, you should rely on blood values and consult a doctor. Hair analyses could provide an indication if you are interested in optimising your diet, but should be viewed critically.
Calcium and the buffer system in the blood:
Calcium not only plays a role in the blood as a mineral for bones, muscles and nerves, but is also involved in maintaining the acid-base balance, albeit more indirectly as a direct buffer. The buffer system in the blood ensures that the pH value remains stable (approx. 7.35-7.45), despite fluctuations caused by metabolic processes or respiration. Calcium interacts here primarily via its binding to proteins and its regulation by hormones
- Forms of calcium in the blood:
Ionised calcium (approx. 50 %): Freely available, biologically active, directly involved in physiological processes.
Protein-bound calcium (approx. 40 %): Mainly bound to albumin, serves as a reserve and influences the pH value.
Complex-bound calcium (approx. 10 %): Bound to ions such as bicarbonate, phosphate or citrate.
The distribution of these forms depends on the pH value and affects the buffer capacity.
- interaction with the buffer system:
The most important buffer system in the blood is the bicarbonate buffer system (HCO₃-/H₂CO₃), supported by proteins (e.g. albumin) and phosphate. Calcium is not a primary buffer component here, but it indirectly influences stability:
pH dependence: with a drop in pH (acidosis), less calcium is bound to albumin, increasing the proportion of ionised calcium. Conversely, with alkalosis (increase in pH), more calcium binds to proteins and the ionised proportion decreases.
Bicarbonate compound: A small proportion of the calcium is present as calcium bicarbonate. Fluctuations in the bicarbonate level (e.g. in the case of respiratory or metabolic disorders) can influence calcium availability.
- Regulation by hormones:
Parathyroid hormone (PTH): When the pH drops (acidosis) or calcium levels are low, PTH is released to mobilise calcium from the bones and increase reabsorption in the kidneys. This indirectly stabilises the calcium level in the blood and supports the buffer function.
Calcitonin: Reduces blood calcium levels if they are too high by promoting storage in the bones.
Vitamin D: Increases calcium absorption in the intestine, which strengthens the buffer reserves in the long term.
- Bones as a calcium buffer:
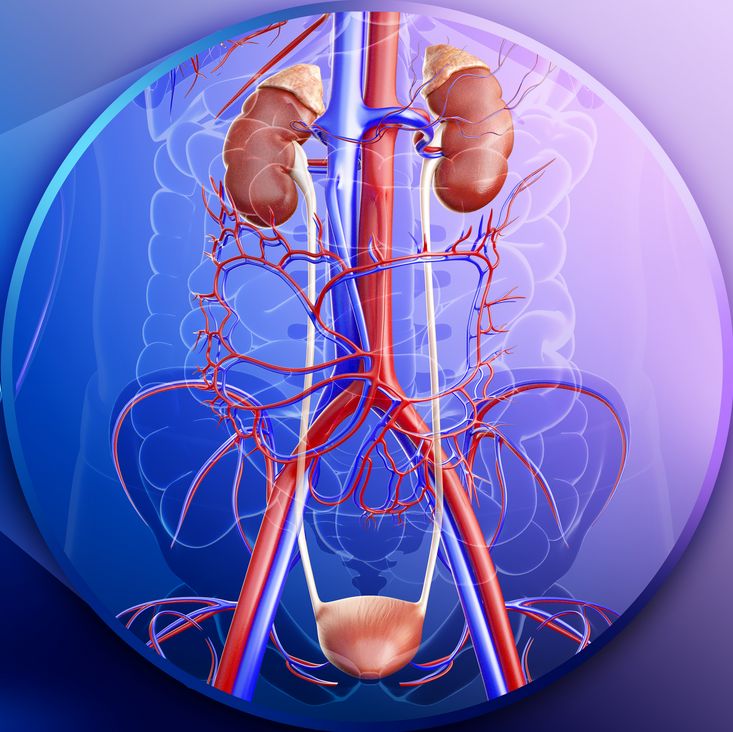
Bones serve as a long-term buffer for calcium and pH. In chronic acidosis (e.g. due to kidney failure), calcium is released from the bones to neutralise excess H⁺ ions. This process provides calcium phosphate, which reacts with acids to stabilise the pH. However, this can become a problem in hypercalcaemia if too much calcium enters the blood.
- hypercalcaemia and buffering:
Too much calcium in the blood (hypercalcaemia) disturbs this balance:
Albumin binding: If the pH drops (acidosis), the high calcium level could be even more ionised, which increases symptoms such as muscle cramps or cardiac arrhythmia.
Kidney load: Excess calcium is excreted via the urine, which can overload the kidneys and lead to calcification if the buffering capacity is impaired (e.g. due to loss of bicarbonate).
Bone loss: With chronically high calcium (e.g. due to hyperparathyroidism), the buffer from the bones is overstressed, which reduces bone density in the long term.
Conclusion:
Calcium is not a direct buffer like bicarbonate or phosphate, but it contributes to the stability of the acid-base balance through its binding to proteins and its hormonal regulation, with the bones playing a central role as an ‘emergency buffer’, while the blood only reflects a small but dynamic part of the calcium.

Too little calcium in the blood, medically referred to as hypocalcaemia, is present when the serum calcium level falls below the normal range (typically <2.2 mmol/L or <8.8 mg/dL for total calcium or <1.1 mmol/L for ionised calcium).
This has a noticeable effect on the body, as calcium is essential for many functions.
Causes of hypocalcaemia:
- underactive parathyroid gland (hypoparathyroidism):
Too little parathyroid hormone (PTH) leads to less calcium being mobilised from bones and reabsorbed in the kidneys.
- vitamin D deficiency: Reduces calcium absorption in the intestines.
- kidney problems: Reduced reabsorption or increased loss of calcium in the urine.
4 Acute conditions:
◦ e.g. pancreatitis (calcium binds to fats), blood transfusions (citrate binds calcium) or alkalosis (more calcium binds to albumin).
- magnesium deficiency: Impairs PTH release and action.
What happens in the body?
As calcium is involved in numerous processes, a deficiency leads to a variety of symptoms:
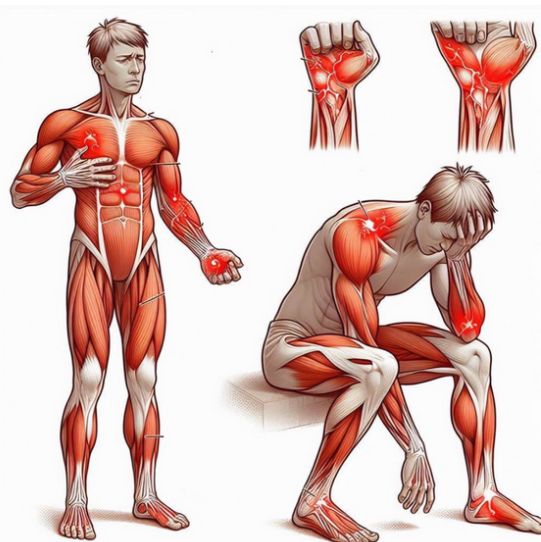
- nervous system and muscles:
Calcium stabilises the membranes of nerves and muscles. If there is too little ionised calcium, these become hyperexcitable:
Symptoms: tingling (e.g. in fingers or around the mouth), muscle cramps (tetany), twitching.
Severe cases: Seizures, as the nerve signals fire uncontrollably.
Clinical signs: Chvostek’s sign (twitching of facial muscles on palpitation) or Trousseau’s sign (hand spasm on blood pressure cuff).
- Cardiac function:
Calcium is essential for muscle contraction, including in the heart muscle:
Effect: prolonged QT interval in the ECG, which can lead to cardiac arrhythmia.
Severe cases: Cardiac arrest if the deficiency is extreme.
- Blood clotting:
Calcium is a cofactor in the coagulation cascade:
Effect: delayed blood clotting, increased tendency to bleed (rarely clinically noticeable as other factors compensate).
- Bones and buffering:
The body attempts to stabilise blood levels by drawing calcium from the bones (via PTH) or reducing excretion:
Short term: bones remain intact as regulation takes effect quickly.
Long-term: Chronic deficiency (e.g. vitamin D deficiency) can lead to bone loss (osteoporosis) or rickets (in children).
- Acid-base balance:
Buffering capacity is indirectly impaired in hypocalcaemia:
Alkalosis: Can increase hypocalcaemia as more calcium binds to albumin and less ionised calcium remains free.
The body does not compensate directly via pH, but an imbalance exacerbates symptoms.
Symptoms at a glance:
Mild: tingling, fatigue, muscle weakness.
Medium: Cramps, confusion, palpitations.
Severe: Tetany, seizures, cardiac arrhythmia.

Compensation by the body:
PTH increase: if the parathyroid glands are intact, PTH is secreted to:
Mobilise calcium from bones.
Stimulate the kidneys to reabsorb calcium.
Activate vitamin D to increase intestinal absorption.
Kidneys: Reduce calcium excretion.
Problem: If the cause (e.g. vitamin D deficiency or parathyroid damage) is not corrected, compensation remains inadequate.
Consequences:
– Acute: muscle and nerve disorders dominate; life-threatening if left untreated (e.g. respiratory muscles affected).
– Chronic: Bone loss, dental problems, cataracts (with long-term deficiency).
Treatment:
Acute: Intravenous calcium (e.g. calcium gluconate) for severe symptoms.
Long-term: Calcium supplements (e.g. 500-1000 mg/day) and vitamin D, remedy the cause (e.g. replenish magnesium).
Conclusion:
Too little calcium in the blood leads to hyperexcitability of nerves and muscles, heart problems and impaired coagulation, as the body cannot balance the level quickly enough. The symptoms depend on the degree and speed of the drop. It indicates an acute regulatory error, not necessarily an overall deficiency in the body – the bones may be full, but the calcium is not getting into the bloodstream, which may also be due to some vitamin deficiency symptoms. What is certain is that we take in more than twice as much calcium through our diet (cheese, dairy products, vegetables etc.) than through water.
Disclaimer: I am not a doctor; please consult a doctor if you need further help.
My personal conclusion, and I speak on behalf of my team, is:
Let’s feel good and grow old as healthily and happily as possible. Laughter is also healthy. Our diet helps us to do this. A large part of it is water, or should be water.
Dear people, drink plenty of water, at least 2-3 litres a day. There is a guideline: 35 millilitres per kilogramme of body weight.
But please, dear people, drink the ‘right water’, namely pure water that is rich in minerals. Because water not only carries calcium, but many other important minerals!!!
https://aguaris.com/en/product-waterfilter/
Many thanks to Frank-Joachim Ehling for this extremely informative article.








0 Comments